Real-Time Monitoring to Reduce Unnecessary Hospitalizations and Improve Patient Outcomes
Background
High need patients cost approximately 17 times more than patients who are not considered “high users” of the healthcare system. There are nearly 12 million adults with high needs, defined as people who have three or more chronic diseases and a functional limitation in their ability to care for themselves (such as bathing or dressing) or perform routine daily tasks (such as shopping or preparing food). As a group, high-need adults used the hospital emergency department (ED) at more than three times the rate of the total adult population. High-need patients were also five times more likely to visit the emergency department for a potential preventable visit.
Providers are seeking to reduce avoidable hospitalizations, which, even with a short length of stay, can cost $10,000 to $30,000 per hospitalization. Nearly 1 in every 5 Medicare patients are readmitted to the hospital within 30 days of being discharged. Annually, $25 billion dollars is wasted on preventable hospital readmissions. Hospitalizations, especially in older adults, can occur for several reasons such as poor quality of sleep, an underlying acute illness (e.g., urinary tract infection), or exacerbation of a chronic illness (e.g., Diabetes).
Providers struggle to identify events or syndromes that progress slowly over time (e.g., cognitive decline, frailty) often have poor demarcation as to onset and transition to new states making the changeover to a new state difficult to recognize. Current assessment practices hinder early detection of critical changes that indicate the onset of chronic conditions, cognitive or functional decline preceding many important geriatric events or syndromes. Current methods make it difficult to identify change or events with detailed temporal precision, intraindividual specificity, and ecological
validity.
Product Implemented in Study
We see our technology fitting seamlessly into the new “ecosystem” of healthcare delivery. Nonnatech’s platform combines passive remote patient monitoring with analytics to detect early signs of patient deterioration. Nonnatech’s platform is a tool to help care managers and others determine if an intervention may be necessary, enabling the identification of patients with a deteriorating chronic disease, non-compliant with medications, at risk for falls or possibly developing an infection. On average 3-5 unobtrusive sensors were setup in the living environments of elderly persons for an average of 6 months. Unobtrusive sensors included bed, chair, toilet, motion, and contact sensors. Nonnatech’s solution provided insights into patient’s activities of daily living, (e.g., eating), mobility, medication adherence, incontinence, toileting habits and sleep patterns. Nonnatech continually processes data through its proprietary health deterioration models that detect and analyze patterns predictive of a hospitalization.
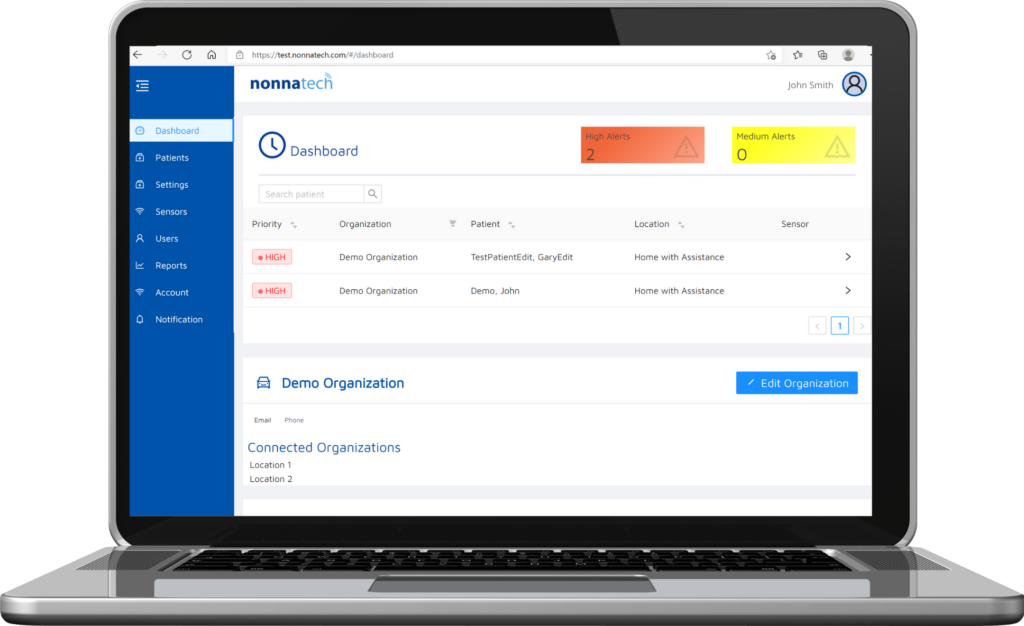
Nonnatech’s platform aggregated the data quickly and accurately, converting the information into actionable information to the care team focused on optimizing resources and performing early interventions. This provided the care team with greater accuracy in identifying deleterious changes in health. Unlike competitive solutions tied to limited use cases in relation to a specific activity (e.g. detecting falls) or a singular chronic health condition (e.g. heart failure), Nonnatech detects meaningful health status changes across a range of chronic health conditions.

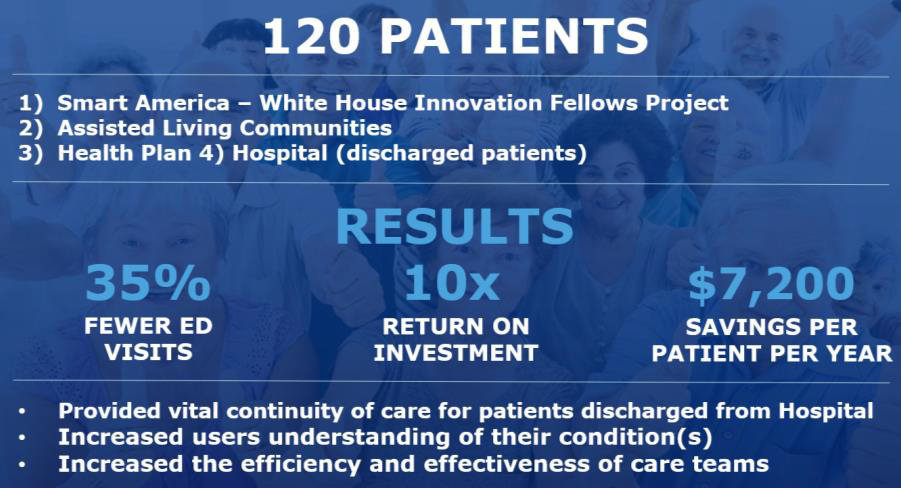
Results
Use of the Nonnatech solution leads to early interventions and overall cost savings. Elderly and chronically ill participants using our solution experienced 35% fewer emergency department visits.
- Provided continuity of care for patients discharged from a hospital or rehabilitation center.
- Reduced an average of 1 caregiver hours per day. At an average cost of $20/hr, this results in savings of over $600 per patient per month.
- Increased the efficiency and effectiveness of care teams.
- Provided staff with necessary information to provide care where needed most
- Staff had more time to deliver more hands-on care as needed
- Reduced number of visits and duration
- Reduced complications with earlier interventions
- Reduced unnecessary visits to physicians, dispatching of nurses or ancillary personnel.
- Allowed participants to remain in their current living environments longer.
- Improved satisfaction across the spectrum of caregivers, families, and residents.
Without Nonnatech, care teams relied on self-reported data from the patient or from a caregiver that many times was incorrect and incomplete. Many alternative solutions also required patients to use wearable sensors and additional invasive methods to collect patient data. In fact, the patient usage rate is less than 15% with these methods. However, with Nonnatech there was no additional burden on the patient, resulting in a participation rate of nearly 90% among participants. We focused on high-risk populations with dementia and additional impairments, which resulted in nearly 90% usage rate. In summary, Nonnatech has demonstrated the potential to impact some of the most difficult and resistant parameters that providers, health systems and health plans face and for which they are now being held financially accountable. Not only does Nonnatech provide enhanced and extended monitoring, it directly impacts the cost and quality of care at a point that is now the most costly “blind spot” in healthcare delivery.
